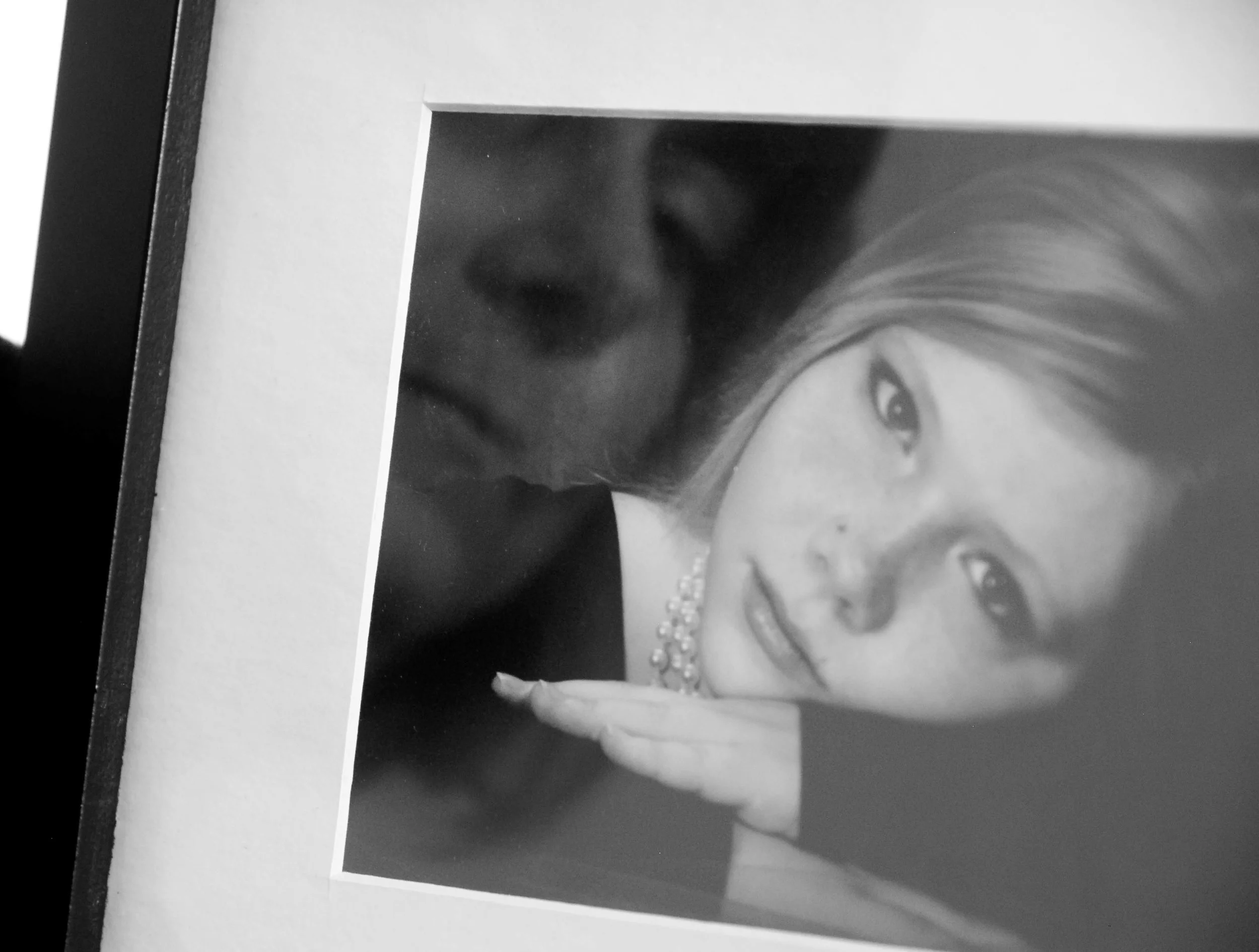
Becky Baker
“The first time I heard about the Stanley Sessions and Whitney Saleski, I was with my daughter, Amanda. We were at a meeting discussing plans for the next National Alliance on Mental Illness (NAMI) KidShop. KidShop is a NAMI program designed for kids in 1st through 12th grade with a mental health diagnosis, and also for kids with a family member with a mental health diagnosis.
Amanda was a trained facilitator for KidShop and I was there as a volunteer. It was there that Michelle Maloy-Kidder, the Executive Director of NAMI of Montgomery County—not to mention our dear friend—told us about Whitney and her Stanley Sessions project.
Amanda was very excited about how this photography project could bring awareness and end the stigma surrounding mental health conditions. She very much wanted to be part of it and tell her story.
Sadly, she is not able to tell her own story now. So, I will be her voice and share her message as seen through my eyes.
On August 12, 2015, Amanda Lynn Baker lost her life to suicide. She was born on April 23, 1989. She was 26 years old when she died.
It has been a year without having her beautiful soul here with me. Some days, the grief is just as strong as the day I lost her…and yet, almost at the same time, it feels like forever since I last saw her lovely face.
Everyone deals with grief differently. For me, it comes in waves. When I first lost Amanda, the waves of grief would pound so hard that I felt I might drown! I learned to let it in a little bit at a time…otherwise, I am sure it would have broken me. It’s a process I am still working on a year later, and I struggle with anxiety now.
One of the hardest parts to process is to know her death was preventable. Suicide can be a symptom of depression and other mental health conditions, just as a heart attack can be a symptom of heart disease. And both illnesses can be treated.
Suicide is not a selfish act. It is a symptom of an underlying illness. People who have this horrendous symptom are some of the strongest, most unselfish people I know. They are fighting every day to stay alive while in great pain.
There are no words to describe the loss of my sweet Amanda. I know there will never be a day that I will not miss her perfect smile, sarcastic sense of humor, and her compassionate and caring soul. When Amanda was 14 years old, she suffered a double whiplash in a car accident. Immediately after the accident, she had pain and symptoms of what we now know to be Dysautonomia.
Dysautonomia is the dysfunction of the autonomic nervous system. It causes many debilitating and painful symptoms, such as severe gastroparesis, syncope (fainting), tachycardia, severe insomnia, and anxiety. For over five years, Amanda saw many doctors who did not understand what was going on with her and would repeatedly refer her to psych. We were told there was nothing wrong with her. Many times, our family was accused of Munchausen syndrome by proxy. The extent of harm this caused over the twelve years she was ill cannot be measured.
Because medical professionals doubted us, the resulting turmoil caused both of us to experience symptoms of posttraumatic stress disorder (PTSD). We actually feared having to visit a doctor or an emergency room. Finally, we found an amazing psychiatrist who not only believed Amanda, but also helped us see a specialist who could diagnose her.
After great difficulty, Amanda was eventually diagnosed with Dysautonomia, postural orthostatic tachycardia syndrome (POTS), severe gastroparesis, idiopathic insomnia, narcolepsy, Ehlers-Danlos syndrome (EDS), immune disorder, MTHFR gene mutation, mood disorder, anxiety, and depression. Treatment is about managing symptoms. This was challenging over the years because her severe gastroparesis did not allow her body process oral medication very well. Her pain, extreme nausea, and sleep deprivation made it extremely difficult to cope and do normal, daily functions.
But when Amanda was able, she would do volunteer work. In 2012, she tried a treatment of ketamine infusions that alleviated her symptoms, including her anxiety and depression. That is when she started working with NAMI. She even spoke in front of the Senate and Congress at the Ohio Statehouse in support of a mental health bill and was instrumental in getting it passed.
In 2014, she was unable to get her ketamine infusions because she had a severe lung infection and had to be hospitalized. Once again, her symptoms worsened—especially her depression—and she began experiencing suicidal thoughts.
Medication was not helping, so in June of 2015, she decided to try electroconvulsive therapy (ECT). It wasn’t easy to find a doctor who would agree to do this treatment because of her longstanding medical issues. At last, we found a willing doctor for ECT, but it was only because said doctor did not believe she had Dysautonomia or POTS! He decided that, after interviewing her for about 30 minutes, she had conversion disorder. Undeterred, Amanda still wanted to try ECT. She had to get a peripherally inserted central catheter (PICC) line for the treatments. After a week of receiving three of the 12 treatments needed, Amanda spiked a fever of 105 degrees. The PICC line caused a blood clot resulting in a massive infection, and she was hospitalized for two weeks. After that, her doctor would not continue the ECT treatments. Once more, her depression grew.
Amanda was always very self-aware. Despite her suicidal thoughts and her struggle to cope, she really did not want to die. She just wanted to live normally and healthfully. I know this because she told me.
She still had hope and believed that her upcoming, scheduled ketamine treatment in October of 2015 would provide some relief. However, she would have episodes where she could not see past the depression and would become impulsive. She was fearful that during one of these episodes, she would harm or kill herself. She wanted to be hospitalized to keep herself safe. Her symptoms of pain, depression, and sleep deprivation were too much for her to handle and she needed support. She would tell me that she did not want to die, but she was afraid something bad was going to happen, and soon.
In the month before Amanda’s death, she tried, unsuccessfully, to get herself hospitalized five separate times.
Each time, she was labeled and dismissed. And each time, no one bothered to try to contact her specialist or even speak to me before discharging her. One time, they flat-out refused to admit her even after she told them she was having suicidal thoughts and had a plan. Two days after being discharged, she attempted suicide by taking too much medication and was taken to the hospital by ambulance. After they got her stable, psych still refused to admit her!
Two other times, they admitted her but then refused to provide the medications that she needed and had been taking for eight years to manage her Dysautonomia. Without one of her medications, she was unable able to eat, and even drinking caused great pain.
At her final hospital admission before her death, they agreed to admit her and put her on a 72-hour hold. Again, they refused to give her medications that were prescribed by her specialists. Amanda tried to advocate for herself, but in the end, was discharged again—this time before the 72-hour hold was up and without talking to me despite my calling and asking to speak to the doctor repeatedly (Amanda always gave consent for medical staff to speak with me).
When I picked her up from the hospital that night, she said to me: ‘we have to do something about this. We can’t let them treat people like this. Do you know how hard it is to admit you need help? Can you imagine how it feels to not be believed or turned away?’
The very next day, during one of her depressive and impulsive episodes, Amanda lost her life to suicide.
Knowing that Amanda wanted to live and fought so hard to stay alive makes my heart ache every single day. Amanda wanted to make this world a better place and tried to be the change she wanted to see in the world. In her short time on Earth, she accomplished so much and made a difference in so many lives. She always had a smile and compliment for everyone even though she was in pain.
She taught me so much and made me a better person. I am very thankful for the time I had with her. My hope is that I can continue to be her voice, help to bring awareness to end mental health stigma, and make much-needed changes to the health care system.
I want to leave you with some of Amanda’s own words. She wrote this in a letter to her grandfather in 2010, and I think it speaks volumes about her character: ‘The person I want to be does charity work but does not want the credit, does the right thing even if no one will ever know, stands up for people who can’t stand up for themselves, and changes the world one act of kindness at a time. Most of all, the most important thing is I want to make you proud of me in everything I do.’”